What is retinal detachment?
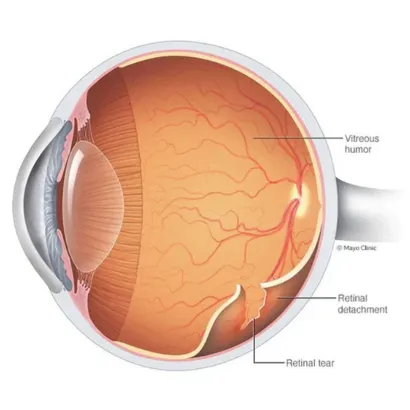
Retinal detachment is an eye problem that happens when your retina (a light-sensitive layer of tissue in the back of your eye) is pulled away from its normal position at the back of your eye.
Retinal detachment is an eye problem that happens when your retina (a light-sensitive layer of tissue in the back of your eye) is pulled away from its normal position at the back of your eye.
If only a small part of your retina has detached, you may not have any symptoms.
But if more of your retina is detached, you may not be able to see as clearly as
normal, and you may notice other sudden symptoms, including:
Retinal detachment is a medical emergency. If you have symptoms of a detached retina, it’s important to go to your eye doctor or the emergency room right away.
The symptoms of retinal detachment often come on quickly. If the retinal detachment isn’t treated right away, more of the retina can detach — which increases the risk of permanent vision loss or blindness.
Anyone can have a retinal detachment, but some people are at higher risk. You are at higher risk if:
Some other problems with your eyes may also put you at higher risk, including:
If you’re concerned about your risk for retinal detachment, talk with your eye doctor.
Rhegmatogenous retinal detachment, the most prevalent type, typically manifests with age. It involves the formation of a small tear in the retina, allowing vitreous humor, a gel-like fluid, to pass through the tear and accumulate behind the retina. This accumulation exerts pressure on the retina, causing it to detach from the back of the eye. The aging process contributes to the shrinkage and thinning of the vitreous, leading to traction on the retina and subsequent tearing.
2.Tractional retinal detachmentTractional retinal detachment is characterized by the pulling of the retina away from the back of the eye due to scar tissue on the retina. Diabetes commonly triggers such detachments, as prolonged periods of elevated blood sugar levels can harm eye blood vessels, resulting in the formation of scar tissue. Over time, these scars, along with areas of traction, can expand, pulling the retina away from its normal position.
3.Exudative retinal detachmentExudative retinal detachment occurs when fluid accumulates behind the retina, even without a pre-existing tear. The fluid buildup displaces the retina from its supporting tissue. Leaking blood vessels or swelling behind the eye, often associated with conditions like uveitis (eye inflammation), are primary contributors to the fluid accumulation leading to this type of retinal detachment.
If you see any warning signs of a retinal detachment, your eye doctor can check your eyes with a dilated eye exam. Your doctor will give you some eye drops to dilate (widen) your pupil and then look at your retina at the back of your eye. This exam is usually painless. The doctor may press on your eyelids to check for retinal tears, which may be uncomfortable for some people. If your eye doctor still needs more information after a dilated eye exam, you may get an ultrasound or an optical coherence tomography (OCT) scan of your eye. Both of these tests are painless and can help your eye doctor see the exact position of your retina.
Your eye care provider will discuss treatment options with you. You may need a combination of treatments for the best results.
Treatments include:
Sometimes, your provider will diagnose a retinal tear before the retina starts pulling away. Your provider uses a medical laser or a freezing tool to seal the tear. These devices create a scar that holds the retina in place.
Your provider may recommend this approach for the right candidates.
During pneumatic retinopexy:
After surgery, your provider will recommend that you keep your head still for a few days to promote healing. Your provider may also tell you what position you should lie in or sleep in. These recommendations may seem uncomfortable or annoying, but they’re particularly important. It’s a short-term sacrifice for long-term benefits.
During a scleral buckle surgery:
During a vitrectomy, your provider:
If your provider uses an oil bubble, you’ll have it removed a few months later.
Your body reabsorbs gas and air bubbles. If you have a gas bubble, you may have to avoid activities at certain altitudes. The altitude change can increase the size of the gas bubble and the pressure in your eye. You’ll have to avoid flying and traveling to high altitudes. Your provider will tell you when you can start these activities again.
While surgery to reattach your retina is often very successful, any surgery can have risks or complications. These risks and complications include:
After treatment for a detached retina, you may have some discomfort. It can last for a few weeks. Your provider will discuss pain medicine and other forms of relief. You’ll also need to take it easy for a few weeks.
Talk with your provider about when you can exercise, drive and get back to your regular activities.
Other things you can expect after surgery:






